Clients or patients facing chronic pain require a special counseling approach that can be applied universally, no matter their source of pain or the number of months or years they have tried to deal with the pain. We have honed and practiced these techniques at the Betty Ford Center in Rancho Mirage, California, because many of the patients we see for addiction treatment also experience chronic pain.
Chronic pain and addiction do not necessarily co-occur, but there are some strong correlations. Unfortunately, because pain medication can be addictive, it is common (but not certain) to find  patients with the combined condition of chronic pain and addiction. All people who abuse alcohol or other drugs experience chronic emotional pain. According to an article published by Jennifer Sharpe Potter and colleagues in the Journal of Substance Abuse Treatment in 2010, chronic physical pain affects approximately 60 percent of those struggling with alcoholism or addiction.
patients with the combined condition of chronic pain and addiction. All people who abuse alcohol or other drugs experience chronic emotional pain. According to an article published by Jennifer Sharpe Potter and colleagues in the Journal of Substance Abuse Treatment in 2010, chronic physical pain affects approximately 60 percent of those struggling with alcoholism or addiction.
At the Betty Ford Center, we have a special treatment program, developed by Dr. Peter Przekop, for both chronic pain and addiction. Regarding chronic pain alone, we have learned several critical counseling techniques that help patients move forward.
Determining if an individual has chronic pain issues
Treatment, of course, begins with an assessment and diagnosis. Sometimes clients or patients will not present their chronic pain as a factor in the reason they are seeking counseling. However, certain markers will help you identify whether the person is dealing with chronic pain. Look for:
1) Symptoms of depression
2) A history of adverse events, including physical abuse, emotional abuse, sexual abuse, a bad accident or a high level of past stress
3) High present stress
4) Anxiety
5) A catastrophizing mindset — a belief that if things can go wrong, they will go wrong
A key part of your assessment is to understand any and all physical pain issues. This detailed inquiry will aid the development of your treatment plan.
There is likely to be related emotional pain as well. Often that emotional pain has early life trauma as its origin. Your assessment and treatment must take this into account. In a national survey of 1,009 chronic pain sufferers completed in 2014 by the Hazelden Betty Ford Foundation, we found a disturbing, though not unexpected, correlation between early life trauma and chronic pain. The chart below lists the top incidents of early life trauma among the survey participants.
One of the most dramatic findings in the national survey was that 97.1 percent of chronic pain sufferers had experienced at least one instance of physical or emotional trauma prior to their chronic pain. We believe this early trauma experience often trains the person’s brain to be more receptive to future chronic pain in a way that does not lead easily to treatment relief. Therapy that helps the chronic pain patient understand, accept and forgive these earlier traumas may help heal the pain center of the brain and make it less receptive to chronic pain.
Counseling techniques
1) Practice being patient with those who are dealing with chronic pain. Inexperienced counselors should know that it is not easy to sit with someone in chronic pain. Many of us in this profession can be caretakers. With clients or patients who have chronic pain, we can tend to want to take away their pain right away. Be prepared instead for a lengthy process. The longer you can comfortably tolerate sitting in session with a client or patient in chronic pain without trying to fix it, minimize it or talk about something else, the more that person will build trust with you. The client or patient will begin to feel that you don’t regard his or her pain as either imaginary or a burden, as the person may have sensed that others have done.
Extended acknowledgment of the pain and listening for the roots of the trauma or concurrent emotional pain builds a capacity within the client or patient for self-exploration and self-awareness. This longer process also helps the client or patient look inward instead of outward, which will benefit the overall therapy process.
2) Offer clients (or refer them to) group therapy in addition to your individual counseling. Unfortunately, a frequent characteristic of people with chronic pain is a tendency to isolate themselves. Because the pain has lingered and feels severe, these individuals talk about it often and intensely with family members and friends. In turn, they have likely eventually experienced being “tuned out.” These clients decide that nobody can relate to what they have gone through. Worse, they may reach an unhealthy conclusion: “My pain is imagined. I’m a wimp. I must be crazy.”
Group therapy, particularly in a community of others dealing with chronic pain, can reduce these clients’ or patients’ sense of loneliness, shame and isolation and help them feel they are not alone. By seeing other chronic pain sufferers who are further along in the process of emotional recovery, your client or patient will gain hope that the day might come when he or she will experience less pain.
Individual counseling provides a different benefit, which is why I recommend both types of therapy concurrently. I begin by recognizing with the patient that pain is pain. By this I mean that our minds and bodies are one unit, and pain will register as pain regardless of whether it is physical or emotional. Emotional pain is just as valid and just as much a contributor to chronic pain as is a medical condition that affects the body. For example, chronic knee pain can be influenced by the pain of unresolved emotional pain.
In this way, it becomes the primary focus of individual therapy to gather information from the client about unresolved emotional pain. As a counselor, you must witness that emotional pain and validate it. Out of this discussion emerges a real gift for the client: a new level of positive self-acknowledgment and self-esteem.
3) Consider adding mindfulness exercises. In addition to traditional emotional counseling, we provide mindfulness training to our patients at the Betty Ford Center who are experiencing chronic pain. Patients spend time in group settings each day becoming aware of how chronic pain has changed their way of thinking, coping and judging themselves and others. Patients learn how to restore normal brain function, in part by working on planned movement exercises that have been taken from the disciplines of tai chi, qigong, kung fu and yoga. Manual medicine and acupuncture also are key parts of the treatment mix. These additional treatment approaches allow patients to learn to refocus attention and help them gain strength, flexibility and confidence. Mindfulness exercises also allow the patients to slow down their minds, control their thoughts and gain a sense of presence. Pain literally steals this ability from people.
Group settings for mindfulness exercises can be helpful as chronic pain sufferers share new skills on how not to focus on the physical pain. Mindfulness helps these patients know where in their bodies they tend to carry the emotional pain from the past. Is it in the same place where they feel the physical pain or elsewhere, such as in the stomach? Patients will come to the realization, for example, that they have internalized and physicalized emotional pain.
4) Help clients learn not to judge the pain. Physical pain is intensified by the person’s judgment of the pain. For example, if your client or patient has a “bad back” and suddenly feels a twinge in the back muscle, that person could spend a significant amount of emotional and mental energy assessing or judging that pain. How much did that hurt? Will it come back? How does it compare with past pains? If you teach clients not to judge or assess the pain, but rather to move on and refocus on something positive, it can actually lessen the sensation of physical pain.
5) Look for signs of chemical addiction. As mentioned earlier, there is, unfortunately, a strong correlation between chronic pain and addiction. Often the addiction is attributable to the pain medication. Your clients or patients may be reluctant to address this issue. I have heard patients say, “I can’t possibly be addicted. After all, these medications were prescribed to me by a doctor.” Or they will say to me, “Addicts live under bridges. I am far from that!” Remember, denial and resistance are typical responses of addicted personalities.
In our 2014 national survey, 48.2 percent of those studied were taking at least three concurrent pain medications prescribed for their chronic pain situation. More than one-third (35 percent) thought they were drug dependent because of the chronic pain treatment. Given that people are reluctant to admit addiction, this number likely is underreported.
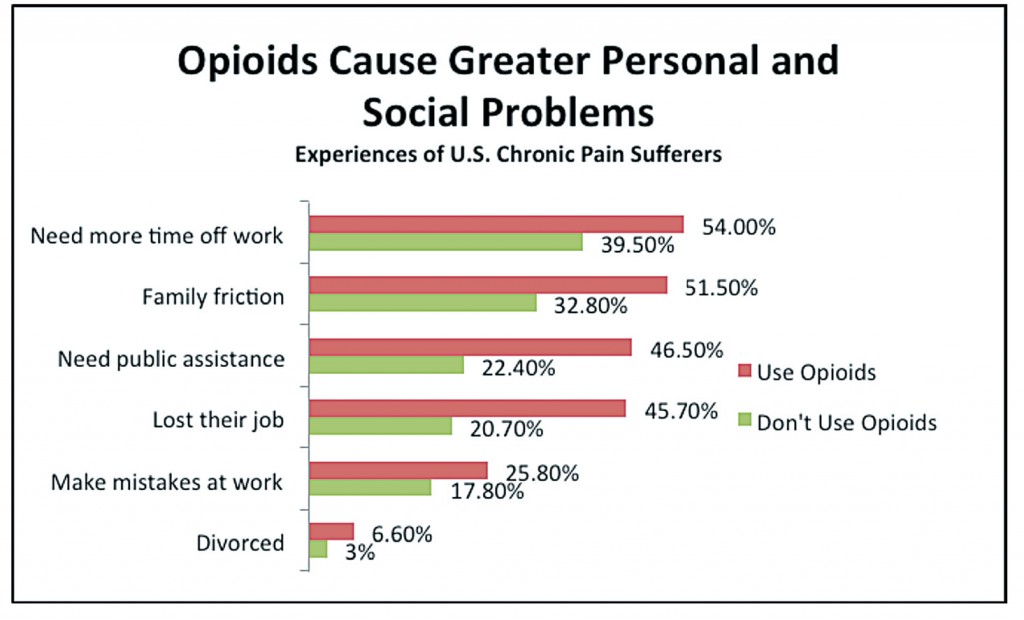 The most common drugs prescribed for chronic pain are opioids, which are highly addictive. Likewise, there are more negative consequences for opioid use than for any of the other prescribed pain drugs. For instance, our study showed that half of patients taking opioids for chronic pain said they had suicidal thoughts. Opioid use (through legal prescriptions) reportedly caused multiple problems that counselors should understand and address with their clients who are dealing with chronic pain. The chart above, taken from our national survey, lists some of those negative consequences.
The most common drugs prescribed for chronic pain are opioids, which are highly addictive. Likewise, there are more negative consequences for opioid use than for any of the other prescribed pain drugs. For instance, our study showed that half of patients taking opioids for chronic pain said they had suicidal thoughts. Opioid use (through legal prescriptions) reportedly caused multiple problems that counselors should understand and address with their clients who are dealing with chronic pain. The chart above, taken from our national survey, lists some of those negative consequences.
6) For follow-up as counseling ends, consider recommending more group therapy. As mentioned earlier, group therapy is an excellent treatment for patients with chronic pain because it puts them in contact with others who are learning ways to cope with the pain. For this reason, after concluding individual counseling with a client or patient, a good ongoing support to suggest would be a chronic pain group.
When making recommendations, avoid two specific types of chronic pain groups. The first is a group in which members are still reliant on medication. We have seen too many patients come to the Betty Ford Center addicted to their pain medication yet still in chronic pain. Medication complicates and often defeats recovery from chronic pain. The second is a group focused on one specific type of pain. In these groups, patients may end up comparing symptoms and aches and pains rather than continuing to move forward with emotional self-exploration and learning new coping skills.
If your clients or patients have chemical addiction issues, I recommend that they participate in a 12-step recovery group. This group will help them focus on recovery from substance abuse, while simultaneously helping them heal related emotional pain issues that pertain to chronic pain.
A proven approach
We use these counseling techniques at the Betty Ford Center. We possess the benefit of treating the patient daily for anywhere from 45 to 60 days, compared with typical counseling schedules of once or twice weekly. We believe this intensity of treatment leads to exceptional results. Retrospective case reviews show that 74 percent of our pain management patients report being free of pain a year after concluding treatment.
This is why we feel so strongly about these suggested counseling techniques for chronic pain. Even if the counseling sessions you provide are less frequent, we believe these techniques will promote healing of the chronic pain and make your clients more emotionally available to address other issues that are causing them difficulty in life.
****
Betsy Farver-Smith holds a master’s degree in addiction counseling from the Hazelden School of Addiction Studies. She has been with the Betty Ford Center for 13 years. Her positions include serving as the executive director of clinical services, and she was recently appointed executive director of philanthropy for the Hazelden Betty Ford Foundation. Contact her at bfarver@hazeldenbettyford.org.
Letters to the editor: ct@counseling.org

Comments are closed.