 Max came into my office and sat down. He was a big guy in his late 30s. When I asked how I could help, he responded that he believed he had posttraumatic stress disorder (PTSD). When I asked what led him to this conclusion, he said he had been a sniper in the military and had been abused as a child. (Author’s note: The name of this client has been changed, but the content is accurate in accordance with his written and informed consent to share his story.)
Max came into my office and sat down. He was a big guy in his late 30s. When I asked how I could help, he responded that he believed he had posttraumatic stress disorder (PTSD). When I asked what led him to this conclusion, he said he had been a sniper in the military and had been abused as a child. (Author’s note: The name of this client has been changed, but the content is accurate in accordance with his written and informed consent to share his story.)
My approach to trauma work has evolved over the years based on what we have come to learn about trauma through research, as well as on my own clinical observations. My therapeutic approach is rooted in client-centeredness, transparency, reverence, compassion and a belief in client strength and resiliency. On the basis of these values, essential components of this approach include accessible language/education, collaboration and evidence-based practice.
When it comes to education and accessible language, the use of metaphors can provide our clients with a much-needed bridge to understanding and normalizing their experiences. Active collaboration with our clients allows them the opportunity to find their power and use it. Because the experience of trauma often involves a feeling of loss of control and having things happen against one’s will, safe and respectful practice requires that clients be informed and willing participants in all aspects of the therapeutic process. And, finally, using evidence-based interventions allows us to provide professional, competent care in helping clients to alleviate their distress, process their trauma and reclaim their lives.
Introduction to the valley of the shadow of death
I often use the metaphor of the “valley of the shadow of death” to explain to my clients the experience of PTSD and the stages of healing. Some clients recognize this metaphor from the Bible’s well-known 23rd Psalm, which begins, “The Lord is my shepherd …” However, its use does not require any spiritual or religious belief on the part of the client or the therapist. I chose 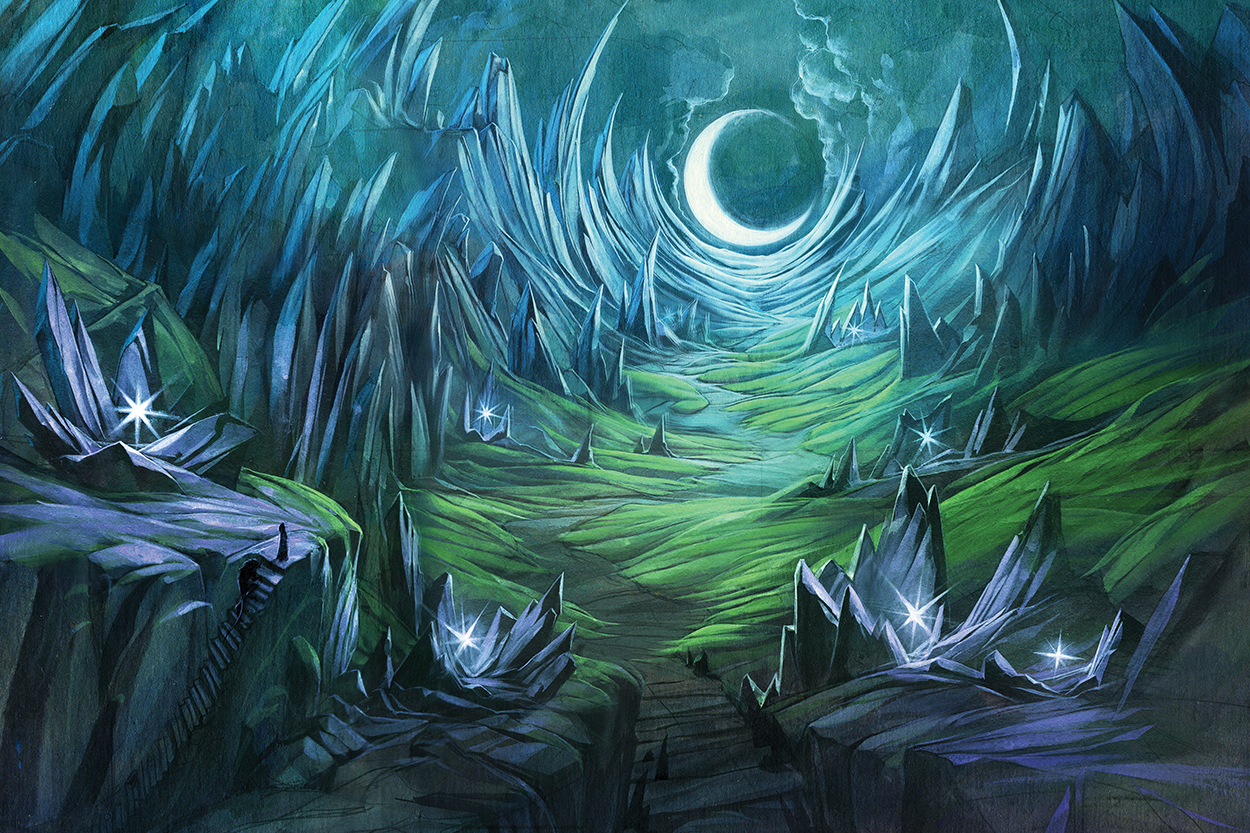 this metaphor because of its power.
this metaphor because of its power.
As I wrote in my book Surviving the Valley: Trauma and Beyond, trauma occurs in “a dark and desolate place that exists in the shadow of some kind of significant ending — a real or symbolic death. In this place, you are apt to feel a profound sense of loneliness, despair and hopelessness. … There are no obvious pathways out of the Valley. The terrain looks treacherous and foreboding. It is difficult to know where to begin.”
In the valley of the shadow of death, the sky is often starless. It can be difficult to recall better times or to hope for them in one’s future. Experiences that send one into this valley typically involve the experience of witnessed, threatened or metaphorical death (e.g., the “death” of trust, innocence, a sense of safety, the belief in fairness or justice). Hope can be elusive.
In my practice, this metaphor has proved to be a powerful means of helping clients find the words to explain what their experience has felt like. I typically introduce this concept somewhere between the first and second phases of trauma work, but I am explaining it to readers here so that the metaphor will make sense from the outset. What follows is the phases of trauma work, explained from the perspective of the metaphor of the valley of the shadow of death.
Phase 1: First things first
Max had never been assessed for PTSD previously. His symptomology was intense. At times, he could be completely dissociated from his body, such as when he walked on a broken leg for a week because he did not feel the pain.
Emotionally, Max was numb. He hadn’t felt emotions for years. He lived his life in survival mode — making him fantastic in a crisis — but Max’s body and mind were always on high alert for threats. He was exhausted, having flashbacks and starting to experience life-threatening medical issues.
We began our work together by assessing and identifying his injuries and normalizing his symptoms. I also started to reflect back his strength, resiliency and courage. At the same time, I was clear with him that he deserved, and would need, external supports along the way. We worked on connecting him with resources for veterans and with medical supports. Max found the metaphor of the valley of the shadow of death to be an apt representation of what he had been living.
****
Once we have determined that our clients are in the valley, we need to identify, assess and begin to respond to their injuries. There also may be crises that require our immediate attention and response.
Some clients will have landed hard in the valley. They may have physical injuries in addition to the psychological ones. Before we even think about moving forward or delving into details of the trauma, we need to identify and assess injuries by asking clients which ones are causing them the most distress currently. (I use the Traumatic Stress Symptom Screening Checklist, which I developed and included in my book Treating PTSD: A Compassion-Focused CBT Approach.) At this point, we can discuss whether mobilizing community, medical, family or peer supports might be helpful to the client. If the client needs help connecting with these supports, we may need to liaise or advocate on the client’s behalf.
Reassurance is a component of this phase. Some clients may be carrying the added burdens of guilt or shame that can come with the misunderstanding that if they were stronger, they would not have ended up in this dark place. Thus, we may need to let them know that traumatic stress reactions are not a result of weakness or character flaws; rather, these are normal reactions to what they have been through.
Given that despair and hopelessness can be part of the symptomology of individuals who find themselves in the valley, checking for suicidal ideation and intent is also essential at the start. If a client is suicidal, it is best we are aware of this at the outset so that we can conduct a risk assessment, create a safety plan with the client and mobilize appropriate resources.
Some clients will not have the strength at this point to hold on to hope. With these clients, I tell them that with all they are dealing with, I recognize that their strength might be lacking, but not to worry because I will hold on to hope for them. I further reassure them that I fully believe we will be able to get them to a point where they can effectively manage their distress and reclaim their lives. (Many of my clients in this situation have responded with relief and gratitude.)
Clients might also be living in unsafe environments that require safety planning or other interventions. This can be another piece of assessing and responding to crises in this phase.
Phase 2: Stabilization and gathering tools for the journey
Throughout the course of trauma work with Max, I provided him with information on how trauma, and specifically complex trauma, can affect the mind and body. He was familiar with the fight-or-flight trauma responses but had not realized that his capacity to respond so effectively in high-risk situations was a result of conditioning through his military training. His experiences and symptoms started to make sense to him, and thus his shame receded.
Max had learned to ignore his physical needs at an early age, which is common with children who suffer from chronic childhood abuse. The first homework assignment that I gave him had three parts to it: 1) to notice when he was hungry and to eat; 2) to notice when he had to go to the bathroom and to do so; and 3) to notice when he was tired and to go to sleep. He smiled when I gave him this assignment and asked how I knew.
Max related to the image of the “warrior spirit” (described further later in the article). Although it had meant something else in his military life, we redirected the energies of his warrior spirit to focus on protecting his healing and well-being.
****
After assessing and attending to injuries and addressing any crises that clients might be facing, it is time to help them get their bearings in the valley and gather the tools they will need for their stabilization and containment — both for use now and on their trauma processing journey (should they choose to take this path).
Some clients will need time to rest and heal before moving on to the next phase of trauma work. We would not expect someone who has just been injured to begin what could quickly become a treacherous climb. Likewise, our clients will need to be stabilized before moving forward in trauma work. They need to be at a point at which they can successfully tolerate or reduce their distress without moving into crisis.
Education is an important component of this phase. Our clients need to know what is normal and what kinds of challenges they might encounter on their journey in the valley. Knowledge about how trauma affects the mind and body can provide our clients with footholds in the valley. We want to help them better understand trauma — specifically, what types of experiences can lead to traumatic stress responses, how people tend to react during traumatic events and the range of normal reactions following such events.
Our clients need to be aware that normal reactions following trauma might include difficulties in the physical, emotional, cognitive and spiritual aspects of their lives. During this part of the work, we are normalizing their reactions during and following their trauma experiences while empathizing with their current distress. It is important that we use easy-to-understand language and concepts in recognition that when our clients are in the throes of severe PTSD symptoms, they can handle only small, personally meaningful pieces of information.
This part of the work also involves helping our clients identify and become comfortable using the tools and resources that will assist them in better tolerating or reducing the distress that they might encounter on their healing journeys. In my work, I have come to recognize 10 such resources or tools to support clients in their journeys.
Within the clients
1) Recognizing their “warrior spirit” within. This involves giving a name to the persona we want to encourage clients to connect with in terms of dual awareness — the strongest, wisest part of who they are that has allowed them to survive the trauma and brought them to this place.
2) Reducing commitments to reduce distress and give clients the time and space to heal.
3) Confronting or advocating with the people, systems, etc., that were involved in causing the trauma in an attempt to address these wrongs or to achieve a sense of justice (when it is safe to do so).
4) Using distraction strategies. These are actions that clients can take to remove themselves from spirals of nonproductive, stress-elevating thinking. Examples: going for a walk, texting a friend, cleaning, drawing.
5) Using mindfulness strategies. This involves moving clients’ awareness from their distressing reliving of past negative events, or their distressing fears of what might happen in the future, to the present moment via the five senses. Examples: noticing a favorite color in the room; feeling the chair one is sitting on; picking up a stone and noticing its texture, color and shape.
6) Using self-soothing strategies. This involves using the senses to calm, soothe or reenergize. Examples: sipping a hot drink, listening to music, inhaling the scents of nature, wearing soft and comfortable clothes, looking at a picture of a loved one.
Through connection with others
7) Seeking counseling support with a mental health professional who specializes in trauma work.
8) Seeking medical support to address physical or psychological pain resulting from injuries or symptoms that are causing distress.
9) Seeking spiritual support from a religious/spiritual leader or peer.
10) Accepting offers of support from caring friends, family members or peers to do household tasks, help with children or take on other responsibilities.
Phase 3: Beginning the climb
Since Max’s life seemed to go from one crisis to the next, it took some time for him to get to a place in which he wanted to start the climb out of the valley. We started with eye movement desensitization and reprocessing (EMDR), but he didn’t want to continue with it because he found the distress that ensued in the days that followed too disruptive to his academics (he was in a college program). Neither did he feel that he had time to do the homework that came with traditional cognitive behavior therapy (CBT). So, I adapted my interventions and created a compassion-focused CBT intervention that we could use in session.
Using a varied approach that met Max’s needs during any given session, we went down many paths together — grief and loss, guilt, shame, anger, dealing with relationship boundaries and so on. Over time, Max began to experience emotions again and had to learn how to manage them. He also started learning to respect his body and its needs. He became very proficient at self-care.
****
Some of our clients will not want to proceed with the journey to climb out of the valley. For them, stabilization and containment will be enough. Given that the climb out of the valley can be life-threatening if people go into it unprepared or unwilling, we should never push our clients to take this step. Trauma is often about loss of control or boundary violations. Healing cannot be. We need to respect our clients’ decisions and inner knowing.
For those clients who wish to proceed with the climb and who appear to be strong enough and well-resourced enough to manage it, we have a number of evidence-based options to offer them. As trauma therapists, I believe we need to be skilled in more than one evidence-based trauma-processing intervention (e.g., EMDR, trauma-focused CBT, CBT). Too often I hear of clients being blamed when they don’t fit with the therapist’s approach. Being client-centered as a therapist means that we need to select or modify interventions to best fit the needs of individual clients.
Often, our clients will need to travel many pathways related to their trauma. These pathways might explore issues of grief and loss, the question of forgiveness of others and self, anger, ongoing depression and anxiety, the adjustment of relationship boundaries and so on. Each individual client’s pathway will be unique. Each individual client will lead. We will accompany, providing a safe, professional alliance and skilled interventions to assist the client in moving through, and eventually out of, the valley.
Phase 4: Living with the scars and reclaiming one’s life
Max became aware of how the trauma experiences he had survived had changed him. He learned to appreciate his resilience, adaptability and survival skills. He also came to acknowledge and embrace the truth of his strength and courage. Through accepting who he was, and is, along with his entire story, Max came to a place of peace.
During our last few sessions together, Max spoke about the newfound sense of peace he possessed. For our final session, I wrote him a letter reminding him of where he had started and highlighting his subsequent successes. I also recalled the qualities in him that I had come to admire. Finally, I reinforced in the letter the message that he possessed all that he needed inside of himself to deal with whatever challenges he encountered, but I reminded him that if he ever needed support again, he knew how to ask for it.
****
Some of our clients will have lived in the valley for several months or years. For these clients, the thought of leaving the valley can invoke both excitement and fear because they will be learning to live in a new way. Thus, the last phase of our trauma work involves assisting clients as they learn to live with the scars (visible or invisible) of their trauma experience; reclaim their lives; acknowledge and celebrate their successes; and move forward on life’s path without us.
PTSD does leave scars, but those scars need to become part of one’s story, not all of it. In this final phase, we work with our clients on how to move forward in reclaiming their power and their lives. Sometimes we will need to assist them in identifying community resources that can continue to support them (such as peer support groups) or causes in which they can become involved that will be meaningful to their healing. Clients living with a disability or chronic pain resulting from their trauma experiences might need a team of medical professionals to provide ongoing support.
This is a time for clients to make conscious and informed decisions concerning how they will move forward in creating their lives outside of the valley. What kind of person do they wish to be? What are their hopes and dreams? Who do they want to have walk beside them on their journey? Do they have certain relationships that need to end or change? These are some of the questions that our clients might explore as they exit the valley.
This final phase is also a time of celebration, kind of like a graduation, as we prepare and plan for the end of the therapeutic relationship. With that being said, some clients will worry about addressing future challenges without our support. In such cases, we can do some role-playing and problem-solving in advance to help alleviate their concerns regarding potential future challenges. For some clients, this might be an opportunity to rewrite their expectations regarding relationship endings. In collaboration with our clients, we can plan how our last sessions will play out.
Somewhere in this phase, we can also take the time to remind clients of where they began in the valley and where they are now, of how they have changed and what they have accomplished. Although this is something we should be doing in each session whenever there is a success, in this final phase we have a chance to summarize all of these successes at one time so that we can both appreciate the extent of their progress. This is often overwhelming for clients — in a positive, celebratory way — as they come to realize how incredible their healing journey out of the valley has been and as they start appreciating the depths of their own strength and resiliency.
****
Knowledge Share articles are developed from sessions presented at American Counseling Association conferences.
Shirley Porter is a registered psychotherapist and a registered social worker who has been providing trauma counseling for more than 25 years. She currently works in the counseling department at Fanshawe College and is an adjunct clinical professor at Western University, both in London, Ontario, Canada. She is the author of two books on trauma: Surviving the Valley: Trauma and Beyond, which was written for survivors of trauma and their support people, and Treating PTSD: A Compassion-Focused CBT Approach, which was written for therapists.
Contact her at traumaandbeyond@gmail.com or via her website, traumaandbeyond.com.
Letters to the editor: ct@counseling.org
****

Comments are closed.