Words matter. The language we use when discussing sensitive, controversial or stigmatized topics reflects and shapes our attitudes and beliefs about those topics. Such is the case with HIV and AIDS. Since being widely identified in the 1980s, HIV and AIDS have been perceived negatively by the general public, resulting in the pervasive use of language that characterizes those living with the virus or the disease as undesirable and even dangerous.
The counseling context is not immune to such damaging language, and it is reasonable to infer that words have a powerful influence on mental health and counseling outcomes for people living with HIV. Counselors must beware of the power of language; outdated information about HIV and AIDS can intersect with the inadvertent use of stigmatizing language and undermine the ethical principles of nonmaleficence and beneficence that form the foundation of our profession. We also have a responsibility to actively oppose HIV- and AIDS-related bias and stigma by educating ourselves about HIV and AIDS and changing the language we use when discussing them.
Let’s start by offering a quick guide to HIV and AIDS terminology:
- HIV: Human immunodeficiency virus; people can be diagnosed with HIV and not have an AIDS diagnosis
- AIDS: Acquired immunodeficiency syndrome; caused by HIV
- CD4 cells: Cells that are a part of the body’s immune system; also known as T cells
- Viral load: The amount of HIV particles in the body
- Opportunistic infections: Illnesses, including certain types of cancer, that occur more often when someone has a weakened immune system
- ART: Antiretroviral therapy, a common treatment for HIV
- PrEP: Pre-exposure prophylaxis, daily medication that can reduce one’s risk of contracting HIV
- PEP: Post-exposure prophylaxis; prescribed use of ART within 72 hours of a possible exposure to HIV
- Viral suppression: When the amount of HIV particles in an individual’s system decreases to the point that the virus is not detectable by current tests; occurs when an individual is adherent to treatment; also known as having an undetectable viral load
The changing face of HIV and AIDS
In the United States, AIDS was originally called GRID (gay-related immune deficiency), and the illness was most commonly associated with gay white males. Although the name of the illness changed as it became apparent that minority sexual orientation was not a determinant of HIV transmission, AIDS continued to be viewed as a “gay disease,” with multiple layers of associated stigma.
Although the stigma remains, the demographics of individuals living with HIV have shifted and increasingly include women and individuals of color. According to the Centers for Disease Control and Prevention (CDC), women account for approximately 20 percent of new HIV diagnoses, and among African American women, the estimated lifetime risk of an HIV diagnosis is 1 in 54 (compared with 1 in 941 for white women). African American and Latinx communities are disproportionately affected by HIV and AIDS. This is largely as a result of social  determinants of health such as access to accurate information, preventive methods and health care, which are influenced by geographic location, cultural and social beliefs, socioeconomics, and stigma about sex and sexuality.
determinants of health such as access to accurate information, preventive methods and health care, which are influenced by geographic location, cultural and social beliefs, socioeconomics, and stigma about sex and sexuality.
As the demographics related to HIV and AIDS have changed since the 1980s, so has the scientific knowledge, leading to key advancements in HIV prevention, diagnosis and treatment. Today, people with HIV can live long, healthy lives, provided that they adhere to treatment and monitor other aspects of their health.
Unfortunately, much of what is commonly known about HIV and AIDS is outdated and inaccurate. For instance, recent surveys conducted by the Kaiser Family Foundation indicated that some Americans still believe that HIV can be transmitted via mosquito bites, shared eating utensils and toilet seats. Many Americans also instinctively associate HIV with death, despite critical advancements in HIV care.
HIV is not a death sentence. For individuals living with HIV, the key to their health is the strength of their immune systems as measured by their CD4 cell count and viral load. Ideally, the goal for people living with HIV is to have a high CD4 cell count and a low viral load. Fortunately, as a result of significant medical advances over the past few decades, individuals with HIV who are consistent in their adherence to ART can have a viral load that is undetectable. Studies have shown, and the CDC has affirmed, that individual with undetectable viral loads have almost zero chance of transmitting HIV to another person even if other protective measures are not present. Never before in the history of HIV and AIDS has there been such hope for HIV prevention generally and people living with HIV specifically.
Unfortunately, not all individuals living with HIV access care and have an undetectable viral load. According to the CDC, approximately 1.1 million Americans are currently living with HIV, with 85 percent of these individuals aware of their HIV status. However, only 62 percent of Americans living with HIV are engaged in care, and only 49 percent of individuals living with HIV have an undetectable viral load. Multiple factors, including public health policies and social determinants of health, contribute to these statistics.
Unaddressed mental health needs might also be at work. People living with HIV may experience adjustment difficulties, depression, anxiety and trauma — all of which can affect an individual’s willingness and ability to seek medical care and remain adherent to treatment. In the past, HIV care focused primarily on the medical needs of people living with HIV. Today, there is growing awareness of the need to address the psychological and emotional aspects of HIV and AIDS because those factors may affect overall wellness.
The power of language
Despite the hope that science has given us with respect to HIV prevention and treatment and the increased awareness of the need for mental health support for people living with HIV, the language frequently used to describe HIV and AIDS continues to bolster the stigma associated with the illness.
Whereas phrases such as “clean bill of health” are benign with respect to other illnesses, when used in connection with HIV and AIDS, they can have a much different connotation. For instance, use of the word “clean” to describe someone who does not have an HIV diagnosis can send the message that those who are HIV positive are somehow unclean and dirty, or even impure and sinful. But HIV is not about clean. Not having an HIV diagnosis is not a determinant of cleanliness or good moral character. Equally, having an HIV diagnosis has nothing to do with being dirty or having loose morals.
Similarly, referring to HIV “infections” rather than HIV diagnoses or transmissions conjures thoughts of contamination, impurity and even death. Simply put, the dichotomy of “clean” versus “infected” breeds stigma, negativity and hopelessness. These negative connotations make getting tested, disclosing one’s HIV status, discussing methods of protection, and accessing and staying in care more difficult.
When counselors inadvertently use stigmatizing language in reference to HIV and AIDS, they risk harming clients by perpetuating stigma and reinforcing barriers to both physical and mental health care. By reducing stigma through intentional language choices, counselors can better help individuals explore their options for entering care or identify potential barriers that may prevent them from staying in care in the future. Additionally, helping clients identify protective factors such as support systems, positive coping strategies and individual strengths can be beneficial to their growth and development.
Regardless of HIV status, and in the name of balance, it is also important for counselors to inquire about aspects of their clients’ sexual wellness when the topic arises. As previously mentioned, with clients who are living with HIV, counselors can discuss getting and staying in care. With clients who are not living with HIV, counselors can use psychoeducation to identify appropriate prevention methods, including PrEP, PEP and proper condom use.
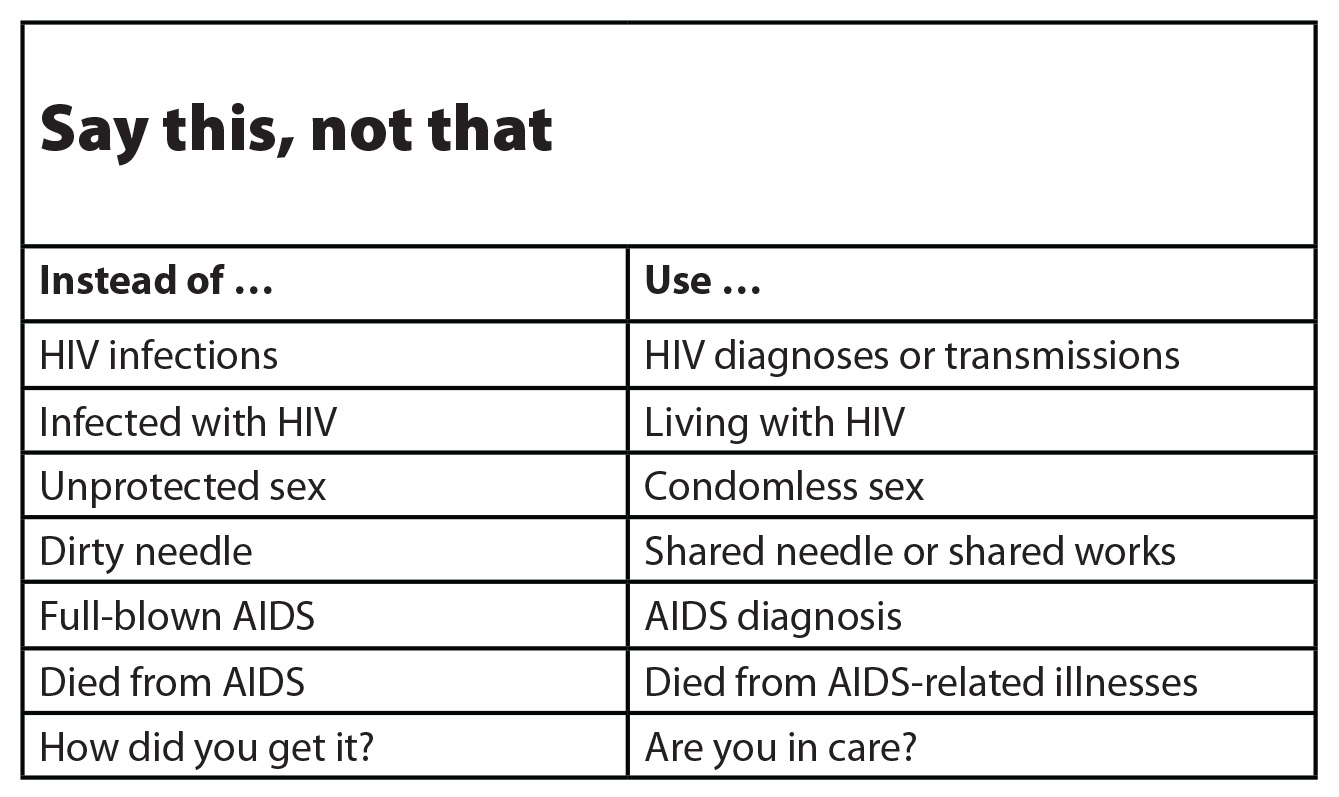
Say this, not that
Recognizing the negative impact that stigmatizing language has on individuals is only the first step toward defusing the taboo of HIV and AIDS. The next step is to identify specific stigmatizing phrases and replace them with appropriate alternatives.
On a foundational level, counselors can make an easy change in their communication about HIV and AIDS simply by using person-first language. Saying “person living with HIV” rather than “AIDS patient” does several things. First, it builds the therapeutic relationship and helps to externalize the diagnosis rather than fusing it with the client’s identity. Second, person-first language decreases stigma by emphasizing the possibility of living, and living well, with HIV.
The use of “person living with HIV” rather than “AIDS patient” also reflects a more accurate understanding of the illness and its progression. Often, HIV and AIDS are used interchangeably, despite an important medical distinction between the two. For counselors, it is essential to accurately differentiate between an HIV diagnosis and an AIDS diagnosis.
An HIV diagnosis follows a reactive test for the HIV virus; however, a diagnosis of AIDS is given by a physician only if an individual’s CD4 cell count is below 200 or if the individual develops certain opportunistic infections. Given that effective treatment is available for individuals who have been diagnosed with HIV, it is likely that someone who is adherent to treatment will never receive an AIDS diagnosis. By ignoring the difference between these two diagnoses, a counselor might appear to be invalidating, deterministic and incompetent to a client who is living with HIV.
Additionally, the phrase “full-blown AIDS” needs to be retired from our collective vocabulary. This phrase — which bolsters fear, reinforces HIV stigma and conjures thoughts of death — is wholly inaccurate and is no longer used among medical professionals. Along the same lines, stating that someone “died from AIDS” is also unproductive and inaccurate. If HIV progresses to the point that an AIDS diagnosis is given, an individual is vulnerable to opportunistic infections, which could be fatal. Hence, an individual might die from an opportunistic infection or an AIDS-related illness but not from AIDS itself.
Accuracy in our language when discussing this particular illness is critical. Errors in our word choices can communicate misinformation and harm clients, adding to the barriers that often prevent clients with HIV from seeking medical and mental health care services.
Conclusion
Understandably, discussing HIV and AIDS can be awkward or uncomfortable for some individuals, including counselors. However, equipped with the right language, counselors can engage their clients in vital conversations about their sexual and mental health. By discussing HIV transmission rather than infection, we can destigmatize the illness and the conversation. We can disrupt the pervasive narrative that equates HIV and AIDS with death, uncleanliness and immorality. And most important, we can be bridges rather than barriers so that people living with HIV will feel encouraged and empowered to access care and live well.
****
J. Richelle Joe is an assistant professor of counselor education at the University of Central Florida. Her work focuses on HIV prevention and culturally and ethically sound services for people affected by HIV or AIDS. Contact her at jacqueline.joe@ucf.edu.
Sarah B. Parkin is a master’s student in clinical mental health counseling at the University of Central Florida. Her research interests focus on intersectionality and marginalized communities.
Letters to the editor: ct@counseling.org
Counseling Today reviews unsolicited articles written by American Counseling Association members. To access writing guidelines and tips for having an article accepted for publication, go to ct.counseling.org/feedback.
****
Opinions expressed and statements made in articles appearing on CT Online should not be assumed to represent the opinions of the editors or policies of the American Counseling Association.

Comments are closed.