In my work with clients with co-occurring mental health and substance use disorders, it became clear to me early on that most have experienced trauma in their lives — trauma that they must resolve to achieve and maintain a healthy recovery.
These traumas are sometimes categorized as little “t” or big “T” traumas. Big “T” traumas include childhood sexual, physical or emotional abuse, natural disasters, war experiences, severe car accidents and rape. Little “t” traumas can be just as damaging, especially because they tend to occur over time and build on each other. This complicates the overall effects of the trauma as well as the trauma treatment. Some examples of little “t” traumas include ongoing emotional abuse or neglect, experiences of shame, being humiliated and being bullied. Incidents involving racism, sexism or homophobia could be classified as either big “T” or little “t” traumas depending on the severity. These traumas might involve one or two distinct incidents, or be more complex, ongoing experiences. The result is a primary belief that the world is not safe. In some cases, individuals who are traumatized learn to expect pain, dishonesty and betrayal from the people they love the most.
In the case of clients with addiction, even if they have not experienced trauma prior to the onset of their disease, they most likely have experienced violence, rage, betrayal, abuse (sexual, physical or emotional), incarceration, homelessness or a whole host of other negative experiences while using alcohol or other drugs.
There are two clinically appropriate strategies for treating posttraumatic stress disorder (PTSD) with people in substance abuse recovery. One strategy is to address the trauma or abuse immediately as the client enters the beginning stages of recovery. The other is to wait until the client’s ability to achieve and maintain abstinence has stabilized.
How do we know which strategy will be successful? Ultimately, the client is the one who knows. If the ability to maintain abstinence from alcohol or other drugs is precarious or impaired due to memories, suicidal ideation or self-harm, it is essential to treat the cause of these symptoms from the beginning. For these clients, recovery will likely remain elusive until their trauma is addressed. If the client is relatively stable, however, waiting until the later stages of recovery is indicated. Clients who are pressured into addressing their trauma issues before they are ready are likely to relapse into active addiction.
According to recent brain research described in Uri Bergmann’s 2012 book Neurobiological Foundations for EMDR Practice, when someone experiences an event or multiple events that cause intense fear, it can change the neural pathways, or maps, in the brain. Whenever something is experienced as a reminder of the trauma, clients can relive that trauma, making them afraid of certain places, tones of voice, objects or even other people with certain body types. Smells can also trigger intense anxiety and fear. The repetitive experience of anxiety and fear can result in panic attacks, health problems, chronic pain, sleeping difficulties and eating difficulties. The individual eventually becomes self-centered, focusing so much on self-protection that there is little objectivity or ability to have empathy for others. This makes every relationship unstable.
 The good news is that several proven therapeutic techniques, including eye movement desensitization and reprocessing (EMDR), can alleviate symptoms stemming from past traumas. EMDR uses the mechanism by which information from frightening and horrifying events is processed into memory and stored in the brain. By manipulating the brain’s intrinsic information processing scheme, a practitioner can help clients release themselves from the intense hold those memories have on them. EMDR combines sensory bilateral stimulation (visual, auditory or physical sensations) with emotional memory and the underlying belief system to lessen the intensity of the experience. It does not erase the memory, but it can reduce or alleviate many of the associated symptoms.
The good news is that several proven therapeutic techniques, including eye movement desensitization and reprocessing (EMDR), can alleviate symptoms stemming from past traumas. EMDR uses the mechanism by which information from frightening and horrifying events is processed into memory and stored in the brain. By manipulating the brain’s intrinsic information processing scheme, a practitioner can help clients release themselves from the intense hold those memories have on them. EMDR combines sensory bilateral stimulation (visual, auditory or physical sensations) with emotional memory and the underlying belief system to lessen the intensity of the experience. It does not erase the memory, but it can reduce or alleviate many of the associated symptoms.
The mystery of EMDR
It is not known precisely how EMDR works, but various research studies have verified its effectiveness in the treatment of trauma. Twenty-four randomized controlled (and 12 nonrandomized) studies have been conducted on EMDR. Most of these studies address simple rather than complex trauma. For a list of these studies, visit the EMDR Institute website at emdr.com and click on the “Research Overview” link under the General Information tab.
In developing EMDR, Francine Shapiro postulated that PTSD is caused by a disruption in the adaptive information processing system. Because the fear and helplessness experienced by clients stays attached to the memory of the traumatic event, it creates havoc in their lives. It is as if the trauma is continuing to happen to them. Because it is still occurring neurologically, it cannot be processed as a memory.
EMDR changes the configuration of the neural connections or map of that event, detaching the dysfunctional physiological and emotional components so that it becomes a more manageable memory. This helps the client “let go” of the past because the neurons are literally letting go of some connections and replacing them with new ones.
In my experience, EMDR is the fastest, most effective and least intrusive way to help clients release trauma, regardless of whether it stems from childhood abuse, sexual abuse or assault, accidents, disasters or combat, and regardless of whether it is the result of a single event or multiple experiences. I have also seen EMDR reduce or eliminate chronic pain, headaches, fibromyalgia and cravings for alcohol and other drugs. One of the best things about EMDR is that it doesn’t require clients to retell their horror stories. In my view, when people don’t have words to describe what they are experiencing, don’t remember the original incident, have somaticized their pain or are too emotionally raw to put the experience into words, it is essential to offer treatment that does not require verbalization.
The eight phases
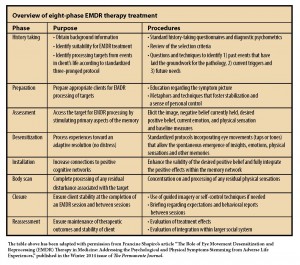
To practice EMDR, a clinician must have a master’s degree, counseling experience and the proper EMDR training. Although the process may seem simple to an outside observer, it requires both an understanding of how the brain and emotions work with trauma and a specific protocol. As shown in the table below, there are eight phases of treatment.
We’ll use “Carrie” to highlight how each phase of the EMDR treatment protocol might be carried out with a client.
- History taking and treatment planning (Phase 1): This is used in most counseling therapies. The therapist and client review biopsychosocial history and trauma history, assess client resources and strengths and determine the frequency and level of any dissociation symptoms. The therapist will suggest different targets and strength-building skills depending on the overall emotional stability of the individual.
“Carrie” comes to the clinic requesting help with night terrors and anxiety. While obtaining her background history, it becomes clear she has survived many traumatic events, has few financial or social resources and is currently separated from her abusive husband. She smokes cigarettes, uses marijuana, uses some mindfulness tools and practices breathing techniques to manage her distress and anxiety. The therapist determines it is essential to improve her emotion regulation and distress tolerance skills, along with targeting various symptoms such as her recurring nightmare.
- Preparation (Phase 2): The therapist explains the adaptive information processing system and how trauma disrupts it. The mechanics of treatment are reviewed. Emphasis is placed on clients nonjudgmentally observing their reactions and awareness, and communicating those observations to the therapist. Rapport is established. Relaxation and self-soothing techniques are taught and practiced.
In Carrie’s case, she is able to best understand the adaptive information processing system with the help of a simple illustration the therapist draws to engage her in the therapeutic relationship. The therapist says, “I will show you exactly what the technique looks like. We can use eye movements, sounds using headphones, or I can tap the back of your hands. Which feels most comfortable to you?” When Carrie chooses eye movements, they arrange the chairs so Carrie and the therapist are facing each other. The therapist holds a pen in front of Carrie and asks, “Is that comfortable? Do I need to change the distance or the pen I’m using? What I will do is wave my pen back and forth, and you follow it with just your eyes.” The therapist does this, and Carrie follows the pen easily.
- Assessment (Phase 3): The client and the therapist determine exactly what the target is, including any images, physical sensations or memories that are associated with the emotionally loaded material. They rate the intensity of the feelings that are attached using the Subjective Units of Distress Scale (SUDS). An “irrational belief” (as defined by Albert Ellis) is identified by the client as the negative cognition. The client chooses a more reasonable belief to use as the positive cognition and rates the perceived validity of this statement.
In Carrie’s case, she remembers parts of her dream: She is in a dangerous situation with people looking for her; she crawls through a hole in a wall to discover she is in a bunker with gunfire all around her. She rates the fear she feels as she recalls the nightmare at a SUDS score of 9. She identifies her belief when these feelings come up as, “I am never safe.” The therapist asks her what she would rather believe.
Carrie responds, “That I am safe, I guess.”
“Are you safe?” the therapist asks.
“No, not always,” Carrie says.
“But sometimes you are safe.”
“Yes, sometimes I am safe.”
The positive cognition becomes “I can be safe.”
The therapist asks, “How true does that statement feel right now?”
Carrie rates it on a Validity of Cognition (VOC) scale as a 1, indicating it feels “like a lie.”
- Desensitization (Phase 4): The cognition, the emotion and body awareness are combined with bilateral stimulation. The therapist changes the bilateral stimulation speed with eye movement, tapping and sounds throughout and between sets. A set is composed of a series of bilateral stimulations. For example, moving the eyes back and forth 10 times would represent a set. The therapist varies the length of a set depending on the intensity of the material the client is experiencing. In between sets, the therapist determines that the process should continue by asking the client if he or she is noticing any changes. This pattern continues until the client reports no change between sets and the SUDS score has been reduced to a 0 or 1.
For example, the therapist tells Carrie, “Bring up that memory, crawling through the hole and being in the bunker. Remember the sounds and smells. Notice how your body feels. Allow the thought, ‘I am never safe,’ to float in your mind. Do not try to direct your thoughts. Let your mind wander. Wherever it goes is where it’s supposed to go.”
Carrie watches the therapist move the pen back and forth, causing her eyes to move from left to right rhythmically. After a set of 10 eye movements, the therapist stops and says, “Take a deep breath. Tell me what you are noticing right now.”
The therapist makes a note of Carrie’s response and starts another series of bilateral stimulations. The process continues until Carrie reports several times that she feels “nothing.” When recalling her nightmare, her SUDS score is 0.
- Installation (Phase 5): The positive cognition is strengthened for the client. The bilateral stimulation is used as the client thinks of the positive cognition. The sets are shorter and slower to allow the positive experience to establish itself. The VOC is measured again until a score of 6 or 7 (“completely true”) results.
- Body scan (Phase 6): The therapist asks the client to pay attention to the way her body feels from head to toe (or vice versa) and report it.
Carrie notices some trembling in her hands. The therapist uses more sets of eye movements until the trembling ceases.
- Closure (Phase 7): The therapist ensures clients are safe to leave the session and navigate their way to their next destination. They are guided through self-calming rituals. The therapist explains that the client may feel spacey or very tired for anywhere from one hour up to a few days. Clients are given an assignment to journal their experiences, emotions, thoughts and dreams until the next session.
- Reassessment (Phase 8): This phase occurs at the beginning of the following session. The targeted material is recalled and the client’s SUDS score is determined. The VOC of the positive cognition is also reevaluated. Any residual processing that occurred between sessions is discussed. If there is a change in either the SUDS or VOC score, it indicates there are more aspects of the target to process.
At Carrie’s next session, she reports the nightmare has not returned. When she remembers it, her SUDS score is 1. The positive cognition, “I can be safe,” is rated at a VOC of 7 (“completely true”).
Conclusion
When I work with a client, I keep meticulous notes about the intensity of the individual’s negative emotions and the perceived validity of the positive cognitions before and after a treatment. I keep this record partly so that I can review it with the client in the future. Many times, the client possesses no memory of having the original problems and emotions. The client still remembers the traumatic incident and has feelings about it, but the incident does not haunt the client any longer.
My experience of utilizing EMDR with clients has been no less than amazing. I continue to be surprised at its effectiveness addressing a number of concerns. It works relatively quickly, and its results are maintained. After the initial setup, it relies on clients’ own processing and therefore validates their experience completely. With EMDR, there is also a shorter period of intense unpleasant emotion that clients experience than with other talk or exposure therapies. It engages the parasympathetic nervous system, leading to relaxation or drowsiness when the process is complete.
Whether EMDR is used at the beginning of addiction recovery or after a period of abstinence, clients are able to manage their recovery more easily and more successfully when PTSD symptoms are alleviated.
****
Jeanne L. Meyer, a licensed mental health counselor, licensed professional counselor and master addictions counselor, is a co-occurring therapist with Choices Counseling in Vancouver, Washington. She is also a member of the American Counseling Association Trauma Interest Network. Contact her at jmeyer@ChoicesCounseling.org.
Letters to the editor: ct@counseling.org

Comments are closed.